What if we viewed lived experience as an asset? As an asset of professional, economic,…
HANs week, tube feeding, TPN and awareness
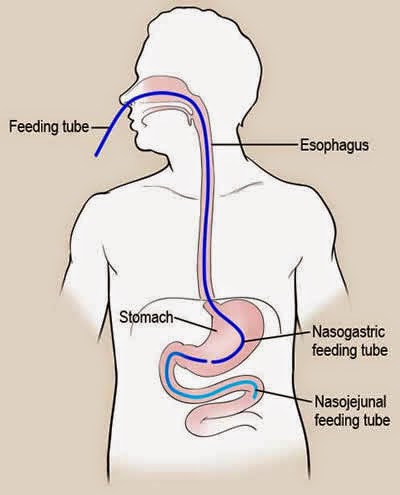
This week is home artificial nutrition (HANs) week. I have been kept alive by artificial nutrition for 5 years. Initially, it was through enteral nutrition, where a special milk is delivered into the stomach or small bowel via a tube, but for the past 3+ years I have been kept alive by Total Parenteral Nutrition (TPN). TPN is intravenous feed delivered into one of the large blood vessels near the heart (or directly into the heart). There are a variety of conditions which warrant the use of artificial nutrition, and they include Short Bowel Syndrome (where the bowel is too short to digest and absorb nutrition properly) caused by conditions such as intestinal volvulus, Necrotising Enterocolitis, Gastroschisis, Inflammatory Bowel Disease, blood clots and trauma, as well as other conditions such as Ehlers-Danlos Syndrome, Gastroparesis, Chronic Intestinal Pseudo-Obstruction and other motility disorders, Crohn’s Disease, Eosinophilic disorders, genetic conditions involving the gut, and short term for any condition which requires bowel rest, such as bowel obstructions and Pancreatitis. There are too many to name, but I hope I have given you an idea of the vast array of conditions that can require artificial nutrition.
 |
| Photo credit: Google |
Enteral feeding has been around for a very, very long time. Enteral literally means “through the gut”. Delivering food into the gut via a tube has been around for centuries. It took a long time before the NG, NJ, Gastrostomy, Jejunostomy, PEG, PEG/J, PEJ and Buttons we know and widely use today were invented, and I daren’t think of all the people who were fed via a tube into the rectum due to the ease of access and quick absorption it provides. Tube feeding originally wasn’t just used for nutrition for those with gut problems, it was also used as an easy way to get drunk – they’d put alcohol up the tube into the rectum and it is absorbed so well and so quickly people get drunk a lot faster (please don’t try that at home!). Once high grade silicon and special plastic tubes were invented and used as feeding tubes, the enteral nutrition possibilities exploded in popularity and have saved countless lives. Unfortunately sometimes they are misused, such as the recent popularity of the “feeding tube diet”, but still, the ability to feed people who can’t swallow, who’s guts don’t work, who need a special elemental feed to give the gut a break from digesting food and to top up people’s nutrition when they can’t get enough from eating, is vital.
| NG feeding |
The main types of tubes are:
NG – NasoGastric, or Nasal Gastric tube, is a tube that goes through the nose and down into the stomach.
NJ – NasoJejunal tube, a tube which goes through the nose, down through the stomach and into the middle section of the small bowel (the Jejunum). This is for people who’s stomach does not work properly and so need the feed and/or medication to bypass the stomach and go into the small bowel.
Gastrostomy – G-tube or PEG, is a tube inserted through the abdominal wall and into the stomach. Some are held in with balloons, others with bumpers or discs. Balloon G-tubes need to be changed regularly, whereas tubes with a bumper (such as the Freka PEGs) can last a few years; my first one lasted almost 4 years.
Jejunostomy – J-tube or PEJ, is a tube inserted through the abdominal wall straight into the small bowel (into the middle section, the Jejunum), bypassing the stomach completely.
G/J – GastroJejunal or Gastrostomy-Jejunostomy tube, also know as a PEGJ, has a tube inserted through the abdominal wall and into the stomach, giving access to the stomach, and through this is a tube which is threaded down into the Jejunum to give access to the small bowel.
Button – buttons are very low profile tubes that lay very close to the skin so you don’t have a tube hanging around unless you are connected. You can’t see them under clothes and they come in G, G/J and J tube types. The most common button makes are the Kimberly-Clark Mic-key tube and the AMT Mini One.
Transgastric-Jejunal – a tube which goes through the abdominal wall into the stomach and is threaded down into the Jejunum.
| My PEG (2009) |
 |
| My PEG and Ileostomy |
I began enteral feeding in August 2009, after losing six stones in six months and getting very malnourished and dehydrated. I started feeding initially through an NG tube, and three months later a PEG was placed and my NG removed. I fed through this for 18 months, and then through a Jejunal extension tube threaded through the PEG and into the small bowel for a few months. I tried many different feeds, high caloric concentrations, fat shots, polycal powder….you name it, I probably tried it Unfortunately I couldn’t digest or absorb the feeds, and I lost eleven and a half stones in two years. I was on so much medication to try and speed up my stomach and bowel, to get it to work properly, but these were unsuccessful.
 |
| 19th May 2011 |
Eventually, after dropping to below 7 stones (consider the fact that I’m 6 ft 1”) and being chronically dehydrated, I was admitted to The Royal London Hospital and was started on TPN. Several days after starting it I had a central line placed. Central lines are tubes which give access to the heart or a large vein near the heart. They either exit on the chest and enter the blood stream in the neck (Hickman line or Broviac) or they exit the skin and enter the blood stream on the arm (PICC line). I have a Hickman line. My Hickman line is what is called a “tunneled line”, where the line is buried under the skin before it exits in a good place on the chest (rather than having a line sticking out of your neck, like the long lines used in hospitals) and the one I have has something called a cuff, which is a bit on the line that the body heals to, holding it in. When dressed, rarely people notice my line unless I have it sticking out. Whereas the PICC is very visible, if you wear a short sleeved top the line is on show. I’m not ashamed of my bags and tubes, but many of us want to keep them low-profile, understandably. Being in a wheelchair makes people stare enough, without having my bags and tubes on show – though some of mine are hard to hide. I have a Hickman line and a PICC at the moment due to having an infection in my line site and we’re not putting my TPN through my line in case there are any bugs in the line; TPN is full of glucose and all the nutrients we – and bacteria – need to survive, so putting TPN through my line when there could be bacteria in it would create a breeding ground and a line infection. All my TPN and meds are going through the PICC, which will be removed in two weeks providing the site infection clears up an there is no infection in the line itself, and only the antibiotics are going through my Hickman line. Next Wednesday we will try putting my TPN through my Hickman line all being well. Home TPN may be referred to as HPN.
 |
| My first Hickman Line |
TPN is a special feed full of all the nutrition we need to survive: glucose, electrolytes, amino acids, lipids (fats), vitamins, minerals and trace elements mixed in sterile water. The amount of fluid in the feed depends on the fluid requirements of the individual, and people get their own “prescription”, and their feed is made to their exact requirements. Some patients are on this for a very short time while recovering from surgery, others short term to build them up or while their bowel needs a rest, and others, like me, rely on it long term. TPN must be delivered through a central line into a big vein because it is very irritating to small veins. When it goes into a large vein or into the heart it is pumped through so quickly that it doesn’t have time to irritate the lining of the circulatory system. Long term TPN is normally a last resort due to the risks and complications. The TPN itself can cause liver problems which, at their worst, can cause liver failure; because nutrition isn’t absorbed through the gut, it is processed by the liver in a different way. The high concentration and different processing of lipids (fats) in TPN can be deposited in the liver, causing fatty liver disease (steatosis). The TPN itself, and the lack of food and normal digestion (for patients that can’t eat), can cause problems with the gallbladder too (cholestasis). Children are particularly susceptible to TPN-related liver disease. Other major complications of TPN are related to the central lines. Line infections are very common, either from bacteria entering the line during connection or disconnection of feed and medication, or spreading from the bowel (translocation). Line infections are very dangerous as the infection can then spread into the bloodstream, causing sepsis (septicaemia). Sometimes IV antibiotics can cure the infections, other times the line must be removed and a new one put in several days later (to stop the infection spreading from the old line to the new one). Blood clots can form on the ends of the central lines used to deliver the TPN to the bloodstream, which can then break off and travel to different parts of the body, disrupting blood flow. Plus there are only so many places you can put central lines, as rarely can you put a line in the same place twice. If people lose lines frequently due to infections or other problems/complications, they may run out of access and without a central line, they can’t have TPN. It is at this point, either repeated infections, liver failure or lack of access, that a bowel or multivisceral transplant (multi-organ, i.e. small bowel and liver; small bowel, liver and pancreas; small bowel and colon etc.) is considered. All that said, TPN is a wonderful thing and without it, me and many others like me would not have survived. We owe our lives to Dr Stanley Dudrick who, despite many doubters, managed to raise beagles, and then keep people alive, on the full range of nutrients needed to survive delivered straight into the bloodstream. TPN has given many of us life, and also quality of life.
 |
| TPN (Vamin, no lipids) |
I have now been on TPN for over 3 years. Prior to TPN I could barely hold a conversation, I was so malnourished and dehydrated and I had no energy. I was tiny and starving to death. Now, though I will say my quality of life is very poor at the moment, for some of the 3 years I’ve been on TPN I’ve had a much better quality of life than I had prior to it. Having my Ileostomy in 2012 also helped. Recent deterioration in my condition has seen my quality of life dwindle but 2013 (and the beginning of 2014) were definitely my years. Speaking in Parliament, winning Friends for Life at Crufts, my ambassadorship with Together for Short Lives and Dreams Come True and all the writing and speaking opportunities I’ve had over the past year have been the highlights of not only the 6 1/2 years I’ve been ill, but my whole life.
 |
| Distention during a pseudo-obstruction |
August is also Gastroparesis (and Pseudo-Obstruction) awareness month. Gastroparesis literally translates as “paralysed stomach”, where the nerves and/or muscles in the stomach don’t work properly and the stomach doesn’t empty normally and so food can sit in the stomach for long periods, even days. This can be accompanied by vomiting of undigested food, pain, nausea and bloating, and it can lead to malnutrition. The term Pseudo-Obstruction means the bowel acts like it has obstructed, but there is no physical blockage. It can cause pain, nausea, vomiting, distention (bloating) and constipation or diarrhoea – things either stop moving and no output is produced or the gut sucks all fluid into the bowel, causing diarrhoea. They are two debilitating conditions. Gastroparesis and Pseudo-Obstruction patients frequently rely on artificial nutrition. Some can eat a restricted diet, others manage on nutritional build-up drinks, some on Jejunostomy feeding (bypassing the stomach completely via a PEG/J or Jejunostomy tube) or PEG feeding straight into the stomach for those whose stomachs can tolerate it, or, as a last resort, patients may rely on Total Parenteral Nutrition (TPN). We also rely on a lot of medications to treat the symptoms such as pain, nausea and the disordered/lack of movement of the gut. Both conditions can lead to intestinal failure, whereby the gut cannot absorb enough nutrition to sustain life.
 |
| In the midst of a pseudo-obstruction, drainage NG, TPN and fluids running, IV Cyclizine administered and still vomiting faeces and no output through my stoma. They are horrendous. |
We are very fortunate that artificial nutrition exists, as it saves so many lives.
Relevant charities and organisations
PINNT – Patients on Intravenous and NasoGastric Nutrition Therapy
PORT – Pseudo Obstruction Research Trust
GIFTUK – Gastroparesis and Intestinal Failure Trust
For the American readers:
Oley Foundation
G-PACT



Just left a comment on an earlier post of yours, after I got to it looking for news about Andy and Lou (of My Last Summer). I read your most recent posts. Good grief. Not much I could say except that you really are going through the mill. Hope you continue to achieve the things you are aiming for.