What if we viewed lived experience as an asset? As an asset of professional, economic,…
NHS Peer Leadership Academy: Day 3 (second residential)
Continuing on with my blog series about the NHS Peer Leadership Academy, here is day three of the Academy. Days one and two took place on 18th and 19th September, and today is day three, tomorrow day four and then days five and six are on the 13th and 14th November. You can read my blog about the first day of the Academy here and the second day of the Academy here. However, here is my blog from Day 3 of the Peer Leadership Academy.
We had another great day today. We began with a hilarious speech from one of the members which showed us how personalised care can really push boundaries and when we think outside the box we can find great solutions.
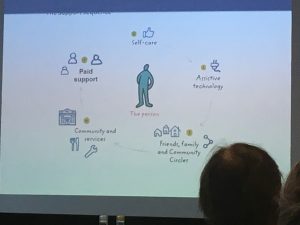
Jo Harvey then gave a presentation on the middle of the triangle of the Personalised Care Operating Model. This supports/applies to approximately 30% of the population. She talked a bit about shared decision making and other personalised care aspects, but focused a lot on personalised care and support planning, what this means, and about self-care. We then had a question and discussion session following on from Jo’s presentation, sharing what some of this means for us, thoughts around this and our experiences and about what changes with people when these components are fulfilled. We were asked to share our experiences and there were some real mixed experiences, however I was able to share how my palliative care team have fully embraced personalised care and support planning, shared decision making and so on, in that when doing my advance care plan age 17, following documenting my end of life wishes, I was asked what I wanted to do with the remainder of my life, however long that would be. I was asked what mattered to me, what my aspirations were, how I wanted to spend my time – no one previously had ever asked me this. So it was nice to share a very positive experience of personalised care and support planning and person-centred care.
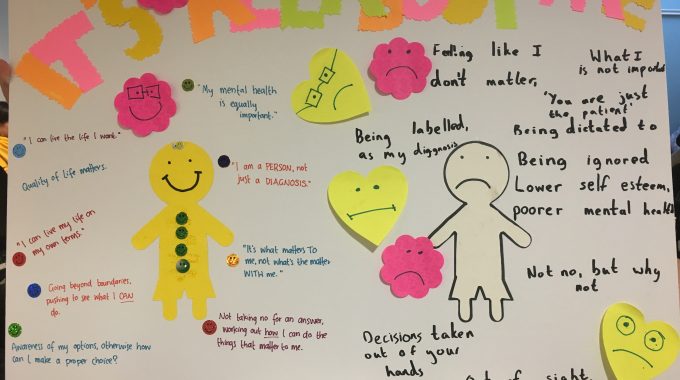
Following a break, we then had an arts and crafts session, in which we had to make a creative poster on what personalised care is. We were split into 3 groups for this. Our group decided to share the impact of personalised care as well as the impact of the lack of personalised care. We had a “happy” side and a “sad” side, with a yellow stick man with a smile on his face surrounded by the positive impacts and aspects of personalised care. This included being listened to, being treated as an individual, being respected as an expert by experience, building our care around us, positive experiences and confidence and self esteem, thinking outside the box, feeling like you matter, being asked “what matters to you” rather than “what’s the matter with you” and having suitable care to be able to achieve your outcomes. On the unhappy side, we had things like not being valued or heard and feeling like you don’t matter and the detrimental impact of this on the person and their confidence, self-esteem and self-worth. We shared about being seen as a diagnosis and not a person and how dehumanising this is. Then at the top of the poster in big multi-coloured letters was “It’s All About Me”.
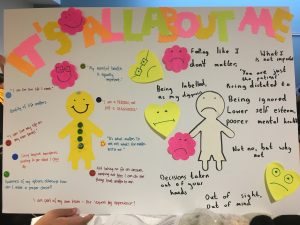
We later presented our posters to the whole group, sharing the happy positive experience and the sad negative experience, and why we did our poster the way we did. and one point I mentioned was that we can, in fact, in one medical encounter be on the “happy” personalised care side, and other times actually be having a negative experience, feeling invisible or fading into the background and feeling like we don’t matter and no one is listening. Each situation is different and especially those of us with many different teams, a positive experience in one doesn’t always mean a positive, personalised experience in the others. I feel our poster was well received and people liked how we’d presented it.
Following the poster creation session, we had another story, this time a lady shared her story of her daughter and how it does take a village to raise a child, sharing the range of professionals involved in her daughter’s care and how she is often the coordinator and communicator. She also talked about her daughter’s PAs being highly skilled professionals, and yet, these care workers are being paid at least £1 less per hour than someone who cleans for Lidls. These are highly skilled staff members and, although that is not begrudging or demoralising cleaners, but effectively her daughter’s PAs are providing intensive care level support round the clock and yet are valued less in society than a supermarket cleaner. I found her presentation excellent and I also love how she related it to the Five Year Forward view too.
After this was lunch and then we presented our posters to the group, before the afternoon session began. Next, Nicola Kay, Deputy Director for Personalised Care Policy and Strategy at NHS England, gave a presentation on the national policy and strategy for personalised care. This was followed by a great discussion with lots of people asking questions and sharing thoughts and experiences.

Then another story presentation, this individual shared his experiences of growing up with a disability and how he felt he lived a very sheltered life as he hadn’t had care independent of his parents until quite late. He also shared about how he didn’t see a future for himself. He shared the importance of early ‘outside’ care for helping young people with disabilities to grow up, and showing young people they have a future.
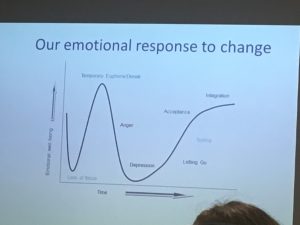
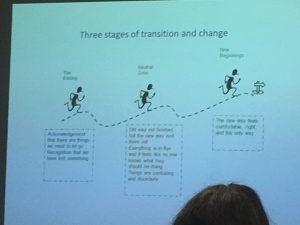
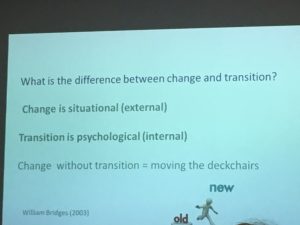
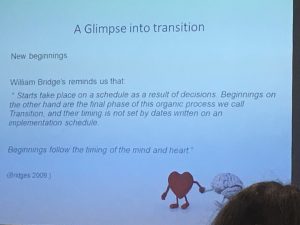
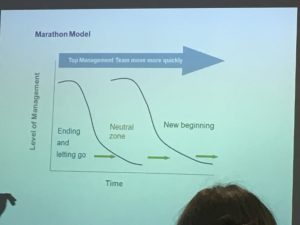
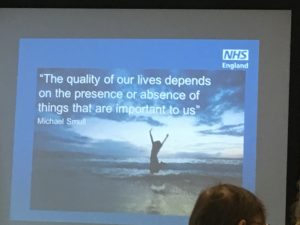
After a quick tea break, it was time for a session led by Steph on change. The message really was that change is internal and external and understanding this and why and how it is so, allows us to be more effective change-makers. She started off by sharing the paradigm shift in the NHS over the 70 years of its existence, and how it was initially about emergency care, not long-term condition care, and how it’s had to evolve, including from professional/clinician-led decision-making to a partnership between professional and patient, how the NHS has split up and devolved and many services are bought-in/subcontracted and how it was previously funded in block contracts whereas now it is subdivided and this includes commissioning on an individual level for Personal Health Budgets and Integrated Personal Commissioning. We looked at barriers in the system and the change management culture – are you an innovator, early adopter, early majority, late majority or a laggard or resistor? We discussed different perspectives on what we are out of the aforementioned and many of us shared a situation where we were a laggard/resistor and what did/would convince us to change. We looked at our emotional response to change and how it is a process, not an action. We looked at the difference between change and transition. Change is external, whereas transition is internal – change is what actually happens around us in the work and the process, where as transition is internal and about our process of personally accepting, moving through and carrying forward change. We looked at the three stages of transition and change: The Ending is first, where we acknowledge that there are things we need to let go of and recognition that we have lost something; Neutral Zone where the old way is not finished and the new way isn’t there yet and everything is in flux and it feels like no one knows what they should be doing and things can be confusing and disorderly; and New Beginnings, where the new way feels comfortable, right and the only way. We looked at the three phases of transition. 1. – letting go – help people acknowledge their losses. 2. – in between time – neutral zone; realigning and adaptation. 3. – New beginning – acceptance and moving forward into new identity and new purpose. We talked about letting go and what health and social care professionals need to let go of. We then looked at the neutral zone in more detail, before going onto the new beginning, including the marathon model. Then a quote was shared that I absolutely love and have used in my work many, many times:
“Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has.” – Margaret Mead
Finally, another story was shared. This related to personalised care and mental health and was very powerful. It made us think about how people with mental health needs are cared for and supported to live well, including not just the active care but the environment too.
Then, that was the end of Day 3 of the NHS Peer Leadership Academy. We later met up for dinner this evening and had great conversations. Now mum and I are getting ready for bed in preparation for another busy day tomorrow.

A very tired out MollyDog!






This Post Has 0 Comments