What if we viewed lived experience as an asset? As an asset of professional, economic,…
NHS Peer Leadership Academy: Day 4 (second residential)
So, continuing my series about the NHS Peer Leadership Academy, here’s an update on Day 4 (aka day 2 of the second two-day residential, the first residential being in September, the final residential being in November). I am now home from Loughborough – or as one colleague of an attendee today pronounced it, “loogabarooga”, which only my fellow Academy members will understand!
We had a great day today, so many thinking points, so much to reflect on and to take on board. I love how it’s challenging me to rethink my thoughts, to see my strengths and think about what I am not so good at and can improve on, and I am learning so much. It’s also been extremely enjoyable listening to the story presentations too – I love stories, I love hearing about other people’s lives, I love seeing another perspective, so that’s been extremely valuable. I am giving my presentation on the final day – I just need to finish preparing it, as with only 10 minutes deciding what is most important to include and what key messages I need to focus on – I could go on and on for ages otherwise – to make my speech the best it can be, and then create the slides to go with it. I am looking forward to getting feedback too. Always an opportunity to improve.
Today started with a quick introduction for the benefit of Zofja Zolna, of NHS England, who was speaking today and collecting stories.
Then our first agenda item for today was a story presentation by a lady who deliberately didn’t reveal her condition so that she would be seen for herself, not her diagnosis. She shared her journey of how a consultation with a specialist consultant who asked her what she wanted, what mattered to her, took time asking questions about her life, hopes, aspirations, interests, work and so on, and then asked her what tools and treatments she’d tried, asked about support groups, asked if there was anything being said in those support groups that might benefit him as a clinician in supporting his patients and so on. He saw her as an individual. She shared the relief and emotion of being valued, listened to, seen as a whole person with a life and when she got upset – happy tears – he gave her a hug. It transformed her from a passive recipient/patient into someone who felt in control of her condition and empowered her to feel like she could do this, be successful and live the life she wants. She shared some great messages.

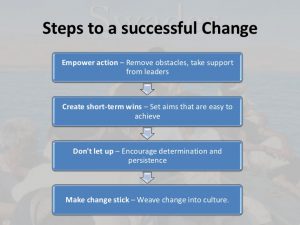
Next Zofja Zolna gave a presentation about a view from the NHS and her story of trying to make a change in the NHS. It was a fantastic presentation, it opened our eyes to the amount of planning, processes, approvals on various levels by various teams and individuals and reviews and justification – and the time – it takes to enable change, and how much determination, persistence, passion, drive, belief and energy is required. She shared the various stages of getting things done and the barriers and hurdles she overcame. She also shared how all the hard work she did at the pilot/demonstrator site ended up falling through, for various reasons, which was difficult, but she was able to carry over all the work she did at that site and replicate it in another site, which proved to be successful. It was very inspiring and empowering – and encouraging to know that persistence is key and that if you persist, work hard, bring individuals on board, inspire those around you and keep believing in the goal/project/change, that you can achieve a successful new programme or change to existing ones. Also that even if you try and fail, that you can learn from it and adapt it, change it, improve it and replicate it elsewhere. I also took a point from earlier discussions at the Academy not related to Zofja’s speech, and that is that sometimes a change being worked for comes ‘too early’ or ‘too late’ – timing is also key. We also talked about innovation fatigue – professionals encounter so many innovations, some successful, others not, and actually if you’re always being sold a new project or a new way of working or a new tool, and have experience of many of them falling foul of their aims, that you become slightly fed up and more resistant and disinterested in innovation as you become fatigued with the constant bombardment of all these innovations and knowing that, in many cases, more fail than succeed. It must be tough. Especially if you’re also having to continuously learn new things, new ways of working, it can become confusing and exhausting trying to keep up with it all.
Following a break, we had a session in which we had to put ourselves in others’ shoes and see others’ perspectives. It was to try and help us understand others’ thoughts, feelings, wishes, experiences, knowledge and their roles, responsibilities and pressures. If we can do this, we will be far more persuasive and effective. Everyone comes at a role, project or experience from a different perspective, we are all unique individuals and we need to understand – and respect – others’ unique experiences, pressures and concerns. I also related this to work I have done around leadership and actually to be an effective leader, you need to understand the group you are leading and their individual perspectives and experiences in order to effectively lead, motivate, inspire, persuade and support your team. For example, through the leadership work I did in another role, I learnt that I am a very coaching and affiliative leader and so I really try to get to know my team and understand their unique needs and perspective and any concerns and worries they may have and work with that, but also visionary in that I can also inspire, persuade and empower them to see where we’re heading – including in that vision, helping to mitigate any fears, worries or concerns they may have. Anyway, I digress. We did some activities around this in putting ourselves in others’ shoes and trying to better understand people we may or do work with.
Next, it was a personal story. This individual shared their story of personalised care with their child, sharing the journey through life from thinking they had to do all of their child’s care themselves, to accepting help, to losing care hours, to fighting for more care, to getting onto Continuing Healthcare and now pursuing a Personal Health Budget. The key message from this speech was we mustn’t underestimate the amount of care given by parents and family members and not to forget carer’s needs.
We had some great discussions over lunch, putting the worlds to rights with a few of the other members, sharing our experiences and talking about different issues such as skilled workers, home adaptations, equipment, getting the care that is needed and the impact of when it is done right, being inpatient when you have complex needs and why there is such a barrier to parents or paid carers caring for the individual in hospital – including saying how ward staff can’t provide 1:1 specialist care 24/7 but also that they do not know the individual well and know what is and isn’t normal and, in the instance of one lady whose daughter who is non-verbal, knowing micro expressions, movements, noises etc. that tell them how she is feeling, what she needs, whether she’s in pain and so on, as is so true of many children and young people, as well as adults, with such needs. We talked about having to travel far for inpatient hospice care and the difficulties of having the “palliative” label and how that is so misunderstood – indeed another lady also shared how she didn’t realise palliative care wasn’t only end of life care, that it was symptom control, supportive care, quality of life, and meeting the person’s medical, personal, social, psychological and spiritual needs, too. It was fantastic as I hadn’t managed to speak to them both before so really enjoyed that opportunity – the social parts of the Academy are as important as the work done in the Academy itself and I am relishing the opportunity to talk to everyone, to hear varying experiences, hear stories, to learn about others’ lives and to gain insight into what life and care is like for others. We are such a broad mix of people and experiences in the group, which makes it even more interesting – you gain so much from talking to others. In my speech at IHUG on Friday last week I talked about how connecting with others, networking, making partnerships and so on is a vital part of making a difference and the change to network and connect with people at events and meetings is equally as important to me as the event or meeting or piece of work itself.
[A slide from my IHUG presentation from Friday 12th October.]
Following lunch, was another story. This story made us think a lot about the impact not only of the right support at the right time, but about the importance and value to individuals of their voluntary, advocacy and campaigning work. It also made us think about how we approach taking time out to focus on ourselves. This individual ended with “Not everyone can do everything, but everyone can do something.” A very poignant quote to end with.

Next we had a session on things not to say – recognising that someone might say or do something that really grinds on us or upsets or angers us, and actually recognising that it’s not always best to actually voice what we are thinking. Recognising when not to say something is equally, if not more important, than recognising what to say and when. We shared some experiences where we’ve had something said or done and have really wanted to say something, but have withheld what we said. We discussed this in our tables and then shared with the group. However our table also discussed why we don’t say these things – and the thing that came out of that, was that almost always it was a fear of negative repercussions or making things worse or with ruining a relationship with someone you have to deal/work with regularly. For me there’s been things my home nurses have said or done that grate on me so bad, but if I were to snap and say something, it would make it extremely difficult and awkward – I am completely dependent on them and need them for almost everything, and I can’t afford to ruin that relationship, nor do I want to, plus I don’t want to upset the other person either. Colin shared a funny story of being in a shop and a man standing slightly in front of him but to the side of the queue. Colin, mentally, was cursing him and saying “If he pushes in front of me in the queue I’m going to…..” and was mentally preparing to have a bit of a go and give him what for, and when the cashier said “next”, this man said to Colin “after you”. Colin felt awful and was so glad he hadn’t said anything. It just goes to show that knowing when not to say something is vital.
After this session, we had another emotional story shared. It showed how one person/professional can completely transform your care – and your life. It was this lady’s first time of sharing her whole story, so was emotional for her. It had such an impact on us all.
Next we had a session talking about boundaries – something that is not my strongpoint and Jo and I shared some laughs about how we both are terrible at saying no to things! We were all asked if we were any good at saying no – no one put their hand up. April did say she’s getting better and it’s about weighing it up with does she value it and is there value to others in doing it and also whether she wants and is interested in doing it. I must say, I am now in a position where I can (and have to) say no to some things. My kind of indicator is when I first read it do I think “Yes I must do this” or do I hesitate? if I hesitate, I need to really consider if I want to do it and if it is valuable to me and others and whether I will enjoy doing it, as there is a reason I will have hesitated. So I am trying to get better. We also discussed the difficulty of feeling obligated – we talked about taking time out to look after ourselves and how others don’t always respect that boundary and keep asking and pleading with you to do something, or keep harassing you whilst you are taking time out. We talked about how hard – but vital – it is to set boundaries. Jo also introduced us to some of the work after the Peer Leadership Academy – some people want to work on the National Strategic Coproduction Group, others want to work on a local level with their CCGs, and others want to work directly with individuals. Also, some people do the Academy and don’t want to move away from what they did already – and that is totally their choice. For me, the difficulty is I want to do all three – national, local and individual work. However I need to weigh up what is most valuable to me and where my contribution will be best utilised. It was interesting hearing about how others have used their role in the Peer Leadership Academy as a stepping stone.
Finally, we did some reflecting on our journey; what resonated most with us, what has made a difference to the way we think or approach peer leadership, and anything else you have gained. For me, I said it was learning new information and having new tools, and then reflecting on these within my own life and work, thinking about my own skills, thinking about how I can improve and about what my priorities and interests are. I felt it’s been a real personal development journey and is benefitting me so much.
Finally, we wrapped up, said our goodbyes and off we went. Everyone was exhausted by the end of it – MollyDog included – and we all look forward to next time. Next time is 13th and 14th November. I can’t wait! But I’ll be sad it’s the last one, too.





This Post Has 0 Comments