What if we viewed lived experience as an asset? As an asset of professional, economic,…

Mid & South Essex Personalised Care & PHB Event – 6th June 2019
Today I co-facilitated an event with the NHS England PHB Eastern Region Lead, Sarah Walker, with the event organised by Sarah, the NHS England Personalised Care Team/Managers and with support from myself. With Essex having one of the lowest uptakes of PHBs and seemingly a lot of challenges and barriers faced in supporting people to have a PHB, and difficulties in getting the process right for every patient, as well as other complicating issues around brokerage and support. We felt we really needed an event to support the delivery of PHBs and personalised care within Mid and South Essex (the Mid & South Essex STP and the individual CCGs within it, Essex County Council, Southend and Thurrock Unitary Authorities, the voluntary, community and social enterprise (VCSE) sector and other organisations and professionals within them). Personalised care is a whole-system approach, so it takes multi-agency, multidisciplinary, collaborative and joint working.
The event was a success, lots of great discussions and questions and I really feel it was a productive event for all concerned – I also learnt a lot today, one never stops learning and I value all the presentations and especially the discussions which bring out such rich information. I hope all the attendees got what they needed out of it and can move forward confidently with PHBs and personalised care.
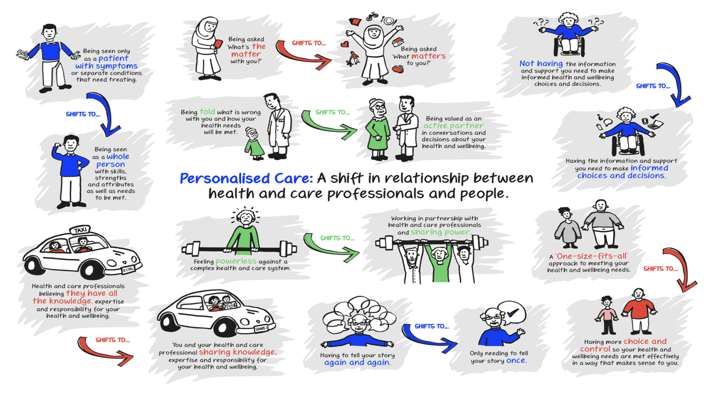
We started off talking about the fact it is What Matters To You Day [#WMTYD19 and #WMTYD2019] today and asking people to think about what matters to them, and I encouraged everyone to keep in mind throughout the event today what matters to them and all the information they get today and the different aspects of personalised care, how that’d be for them, what a good PHB would look like for them personally, and how things would make them feel. We then went straight into the presentations. Jennie Walker (NHS England) introduced us all to personalised care, the comprehensive model of personalised care and the operating model, and talked about things in the context of the NHS Long Term Plan, and then talked about “Bringing The Model To Life”. She went on to speak about shared decision making, personalised care and support planning, supported self-management and patient activation (and the Patient Activation Measure). I contributed my experiences (briefly) into the personalised care and support planning aspect. Sian Brand gave a fantastic presentation about social prescribing, Jim gave a great presentation about finance, commissioning and contracts, and then Helen Farmer and Stevie Attree presented on examples from Thurrock. Myself and Sherone Phillips presented on strategic coproduction and Sherone touched on workforce, and we did an exercise around the shift in relationships that personalised care enables, and how this can be achieved. I then shared my experiences of Personal Health Budgets and we then had a useful presentation by Sarah sharing the numbers from the different CCGs for the different types of Personal Health Budgets and integrated budgets, and did some activities about how we will improve our practise moving forwards. A very useful event, a lot of information shared and some fantastic questions and discussions, I often find discussions following presentations to be the most useful bit, as it’s when people translate what they’ve just heard/learnt and process it, try to understand it and then see what they can do to utilise/implement it.
In the personalised care and support planning part when I shared my experience, I talked about the process of doing my personalised care and support plan in the early years, and how, since then, I’ve updated it largely myself without the need for a multidisciplinary meeting (MDT) but the difficulty I find is that I have lots of different plans with different organisations and/or services. I described having multiple plans with multiple professionals, my personalised care and support plan with the Continuing Healthcare (CHC) team, my district nurse care plan, my hospice care plan, my personal home care plan, my advance care plan etc. and how it’d be so much easier if these were amalgamated into one plan that everyone worked from (albeit I still feel the advance care plan should be separate as well as integrated into the personalised care and support plan). I was asked why I couldn’t just have one plan, and I explained that everyone wants a care plan written by them, owned by their organisation and on their own letterhead and care plan template, and I have suggested trying to amalgamate these, but as yet it’s never materialised. Another person said about why we don’t use technology like Skype or Zoom to hold multidisciplinary meetings as then everyone can be metaphorically “round the table” but without physically needing to travel to a location, and why this isn’t utilised more – it would make such a difference for patients and carers, and indeed the professionals working with us.
A bit later I co-presented on strategic coproduction, which we had to keep very brief, with Sherone and Sherone shared parts of the model around coproduction and workforce, and I shared about my experiences of being a member of the national Strategic Coproduction Group, what it means to have people with lived experience on board, how it’s about collaborating, working together, supporting each other and using patients’ lived experience to improve services, systems and processes, and can translate into other work on other projects, for example coproducing care or commissioning models, or a new care plan template, for example. Sherone went onto say that many people are scared to involved people with lived experience and how actually, not everyone is suited to being a member of a strategic coproduction group, you can’t have people with an axe to grind and who comes from a place of “this is wrong and I am going to keep complaining until it’s put right”, these individuals need to be able to harness their lived experience and then have a detailed knowledge of the system, processes, policies, frameworks, the culture and the hierarchy/structure in order to work collaboratively, coproduce and co-create care and improvements to the health (and other) services, and how it takes investment in people to help them to learn the systems, culture, policies and so on in order to be able to work strategically, work equally alongside professionals, to know how to get on with and work with professionals and to utilise your lived experience but equally be able to step outside it and contribute to strategic work. Sherone and I had a conversation about the notion of “representation” and how people like me don’t represent anyone, rather we’re a person with lived experience who can bring the knowledge and experiences of others to the right table at the right time, but no one person or group of people, can represent other people. Sherone and I had also discussed the fear around involving people with lived experience and how often professionals feel they cannot be honest about the service and care if there is a “patient” or “carer” present in the room, when in fact this is the perfect place for learning and collaboration, and of course, coproduction. I shared my desire to start up a strategic coproduction group in Essex for Mid and South Essex STP in particular, and received a lot of positive responses from nodding heads to various conversations. Following this some questions were asked and statements made including from a commissioner within social care who is setting up a coproduction group/network for their work, so whether there is potential for collaboration or combining our work into one group, we’ll communicate separately and see what we can do in partnership.
In the afternoon session I shared my experiences of Personal Health Budgets. I shared the overwhelming positives, and few negatives, in my experience of having PHBs. I went back to 2013 when I became one of the first in Essex to have a Personal Health Budget and how the package was somewhat inadequate and relied almost completely on my mother to do most of my care and to do all of the nursing/clinical tasks 24/7 without support. I described how we fought to get it so that mum was paid to administer one of my infusions per day so mum could give up work and care for me, and I could have my nursing needs met in the community, as it was clear no actual funding for nursing was going to be granted. Then, in 2015, mum was diagnosed with a brain tumour. We fought for a package of care in which we had 3 weeks to build a very complex 24 hour package of care, but my CCG pulled out all the stops and got it instituted so mum could have her surgery. It was here we discovered there was no contingency in my PHB – I should’ve had a solid contingency plan for what if mum became ill or injured and what care would be provided as an emergency, but no such plan existed – everyone had always relied on mum being able to do all my nursing care round the clock. However I got the 24 hour package and mum had her operation, but suffered severe complications so this interim package was made permanent; soon after we knew it was going to be permanent, I posed the question, “Can I have a Personal Health Budget again?”. So we began making the preparations. It took a further two and a half years for Phase 1 of my Personal Health Budget to be realised and started, for the overnight care and the 6 hours of double-up care alongside the nurse, so I could employ my own PAs. Once again, I fought for mum to be paid on my package – having made a miraculous recovery considering she wasn’t expected to survive, and now being fit and well enough to do so – to provide most of the 2:1 care alongside the nurse so I didn’t have to completely fix my hours and lose any ability to live my life, as my routine changes hugely day to day and I have no fixed routine for when I need those 2:1 hours, but mum is happy to work round me and so I made a case to the CCG and was successful – an example of them personalising their processes and policies to best meet my needs, the needs of the patient/person. Currently we’re in the process of setting up Phase 2 in which my 16 hours per day nursing care will be moved onto the PHB. I cannot wait to have total choice, control, flexibility, freedom and autonomy again over my life and my care. This speech received positive feedback and I hope people took a lot away from it. No, my PHB experience wasn’t perfect, but despite the issues with the first PHB falling apart, I still rate my experience of PHBs as very positive. They are transformative and the only way I can truly live my life to the fullest, do my work and contribute to society, as well as to have fun, achieve my goals and make precious memories. I also touched on how transformative PHBs are and what they mean for – and to – me and others like me, those who sit at the top of the triangle on the Comprehensive Model of Personalised Care in the top 5%, although PHB use is expanding. I also shared in my speech my delight that in 2018/19 we reached 54,143 people benefitting from a Personal Health Budget, a huge achievement, so we all applauded ourselves, all the professionals working hard and the NHS England teams for reaching this stage 2 years before the mandate. We gave a few cheers to celebrate this achievement.
Individuals from the Clinical Commissioning Group that support me, Castle Point and Rochford CCG (CP&R CCG), were present today including my Continuing Healthcare nurse and the Head of Care. My CHC nurse is fairly new to me (since January 2019) but the Head of Care has been involved closely in my care for a few years and was instrumental in Phase 1 of my Personal Health Budget (overnight care and double-up care) being set up and that care moved from the agency to the PHB – she went over and above her job role and had a lot of intensive contact with me and my case even though that isn’t her job and so she is a big part of the reason my PHB finally went ahead, and now my CHC nurse is supporting me through the process and working with me to get the nursing care moved from the agency onto my PHB so I can employ all my own staff, both nurses and PAs, and have total control over my 24 hour care.
A very positive event that I felt went very well. I look forward to collaborating with others and hopefully setting up the strategic coproduction group, and supporting the CCGs to involve people with lived experience and to improve their processes, the system, the service provided and the outcomes for people and their families. I can truly say, I love my “job”. It’s a privilege to work nationally with the NHS England Strategic Coproduction Group, and on the NHS Assembly, but I am looking forward to making an impact locally, too.
Key people and accounts to follow on Twitter:
NHS England Personalised Care Group @Pers_Care
NHS England Personal Health Budgets Team @NHSPHB
James Sanderson, Director of the Personalised Care Group at NHS England @JamesCSanderson
Sarah Walker, Eastern Region PHB Lead @SarahWProjects
Jennie Walker, Personalised Care Group – Personal Health Budgets Lead and Midlands and the East Regional Lead @JennieWalkerPC
Sherone Phillips, Manager, NHS England Personalised Care (Lived Experience Team) @SheroneHD
NHS England @NHSEngland








This Post Has 0 Comments